MILWAUKEE — Over the past two years, the scientific world has seen a steady flow of research updating what we know about the novel coronavirus, SARS-CoV-2, and how it affects humans.
What You Need To Know
- The omicron variant is linked with a lower risk of hospitalization, which may be because it's not as good at getting into the lungs
- Rapid antigen tests may not catch omicron infections in their early days, even while people are contagious
- COVID-19 vaccines don't increase birth complication risks, but catching the virus does — especially for the unvaccinated
- Pfizer's vaccine is highly effective at stopping MIS-C cases in kids
Because the virus is so new, researchers are still grappling with many questions about its function. And because of the nature of the scientific process, no single study can completely answer those questions. Instead, new research is constantly challenging our understanding of the pandemic.
Here, we explore some recent studies that have shed new light on the virus.
Omicron linked with lower hospitalization risk, less lung damage
With omicron making up just about every new COVID-19 case in the U.S., according to CDC data, experts have been working hard to understand key questions about the latest variant to sweep the world.
A silver lining amid the surges: More evidence has suggested that omicron infections have a lower risk of hospitalization, compared to other versions of the virus.
A preprint study out of California last week found that, stacked up against the delta variant, omicron was less likely to cause severe disease. Omicron-infected patients were around half as likely to be hospitalized, compared to those infected with the delta variant, the researchers found after looking at records from around 70,000 COVID-19 patients.
Even if omicron patients were sick enough to head to the hospital, they usually didn’t stay as long, the study found: The omicron variant cut the average hospital time by three days, or 70%, compared to delta infections. Omicron patients were also less likely to die, or be put on a ventilator, compared to delta patients.
Across the world, other studies have painted a similar portrait for the new variant. From South Africa to Scotland, Texas to England, research teams have found that omicron is linked with a lower hospitalization risk, compared to past variants.
Some research in the lab has given us clues as to why omicron cases are, on average, less severe.
Studies have looked at how the new variant behaves in mice and hamsters, as well as in human tissue. What they’ve found is that omicron seems less effective at attacking lung cells, and instead tends to stay more in the upper airways like the nose and throat.
These findings suggest that “the virus establishes a very local infection in the upper airways and has less chance to go and wreak havoc in the lungs,” virologist Melanie Ott told Nature.
In hamsters, for example, omicron showed up in the lungs much less than other versions of the virus — but it still had similar levels in the nose, one study found. And the hamsters tended to get much milder symptoms with omicron: Their lungs weren’t as damaged and they didn’t lose as much weight.
Of course, even a virus that’s technically milder can put lots of people in the hospital, especially one that’s as contagious as omicron. As the new variant’s cases have surged, hospitals have still faced overwhelming numbers of COVID-19 patients, many of them unvaccinated.
“Since it’s more transmissible, there will just, at some point, be a lot of hospitalizations that inevitably occur,” epidemiologist Joseph Lewnard, an author on the California study, told The New York Times.
Rapid tests may miss some omicron infections early on
With long lines at test sites and long waits for lab results, rapid tests have become a key piece of our COVID-19 testing strategy.
But recent research has shown that the rapid antigen tests, including at-home kits, may not catch cases in the early days after an infection — even when patients are carrying enough virus to get other people sick.
A pre-print study from this month focused on a handful of workplaces that were monitoring people every day with both rapid tests and lab-based PCR tests. The researchers compared PCR and rapid results for 30 employees who were infected with COVID-19 during omicron outbreaks — who were vaccinated and, in many cases, boosted.
In all of these cases, the rapid tests kept showing negative results after the PCR tests caught the infection. On average, it took three extra days for rapid tests to catch the infection after a positive lab test, according to the study.
We’ve long known that PCR tests are more sensitive than rapid antigen tests, and can catch a COVID-19 infection while the virus is still at lower levels.
But the researchers also found that in 28 of the 30 cases, rapid tests were still turning up negative results even when viral levels were high enough to infect other people. In four cases, the scientists confirmed that patients passed on the virus to others while they were still showing up as negative on rapid tests.
The study’s authors concluded that “most omicron cases were infectious for several days before being detectable by rapid antigen tests.”
Scientists are still trying to figure out why rapid tests are missing some of these early cases, especially with the now-dominant omicron variant.
Experts told STAT News that the difference probably comes from how omicron behaves in the body — not because the virus has mutated too much for tests to recognize it. Some research has suggested that throat swabs can help catch omicron infections.
“I think that with every new variant that comes, scientists have to question whether the things that were previously true are still true,” study author Blythe Adamson told STAT News. “This one has a different way it travels, a different mechanism of action of symptoms, it has different windows of transmission.”
It’s not all bad news, though: Another recent study suggested that a popular at-home test kit — the Abbott BinaxNOW version — still does a good job at catching the most infectious omicron cases. The rapid tests caught 95% of COVID-19 cases with the highest viral loads, and did especially well for patients who had symptoms, according to the study.
COVID-19 vaccines don’t raise risk for birth complications — but COVID-19 disease does
Early on in the COVID-19 vaccine rollout, health officials were less sure of whether to recommend the shots during pregnancy, since there wasn’t much data from clinical trials.
But that picture has since changed. Health experts now urge expecting mothers to get their shots, as more and more evidence has shown that vaccines are safe — and that COVID-19 is very unsafe — during pregnancy.
A study from the CDC this month found that women who got vaccinated for COVID-19 while pregnant were not more likely to give birth prematurely. They also weren’t any more likely to deliver babies who were underweight, the study found.
Preterm birth and unusually low birth weight are both linked with long-term health problems. But the 10,000 vaccinated mothers in the study — most of whom had gotten a shot in their second or third trimester — didn’t see any higher risks of these complications, compared to the 36,000 unvaccinated mothers in the study.
Earlier studies had also found that COVID-19 vaccines were not linked with higher risks of miscarriages or stillbirths. The new findings “add to the evidence supporting the safety of COVID-19 vaccination during pregnancy,” the study’s authors wrote.
On the other hand, getting infected with COVID-19 while pregnant is a big threat to both mother and baby, especially for the unvaccinated, as recent research has highlighted.
A study out of Scotland this month found that women who contracted COVID-19 during their pregnancies faced higher risks of preterm birth, stillbirth and newborn deaths.
For women who gave birth within a month of their COVID-19 diagnosis, the outcomes were especially bleak: They were around four times more likely to lose a baby to stillbirth or in the first month of life, and around twice as likely to give birth prematurely, the study found.
And most of these severe outcomes — including all of the baby deaths — occurred in women who were not vaccinated, researchers found.
“Vaccination in pregnancy is the safest and most effective way for pregnant women to protect themselves and their babies,” study author Sarah Stock told STAT News. “This advice needs to go out to partners and parents and grandparents and friends.”
Despite these risks, vaccination rates during pregnancy are still far behind the general public. Around 42% of pregnant adults were fully vaccinated as of CDC data this month, compared to around 63% of all Americans.
More news to note
Pfizer’s COVID-19 vaccine is highly effective at preventing MIS-C — a rare but serious inflammatory disease — for kids who get infected with the coronavirus, according to new CDC research. The shots helped cut MIS-C risk by 91% in those aged 12 to 18, the study found.
Our genes may offer a clue to why some people lose their taste and smell during a coronavirus infection, according to a study this week. Researchers from 23andMe found that a certain genetic risk factor may be linked with these signature symptoms of COVID-19.
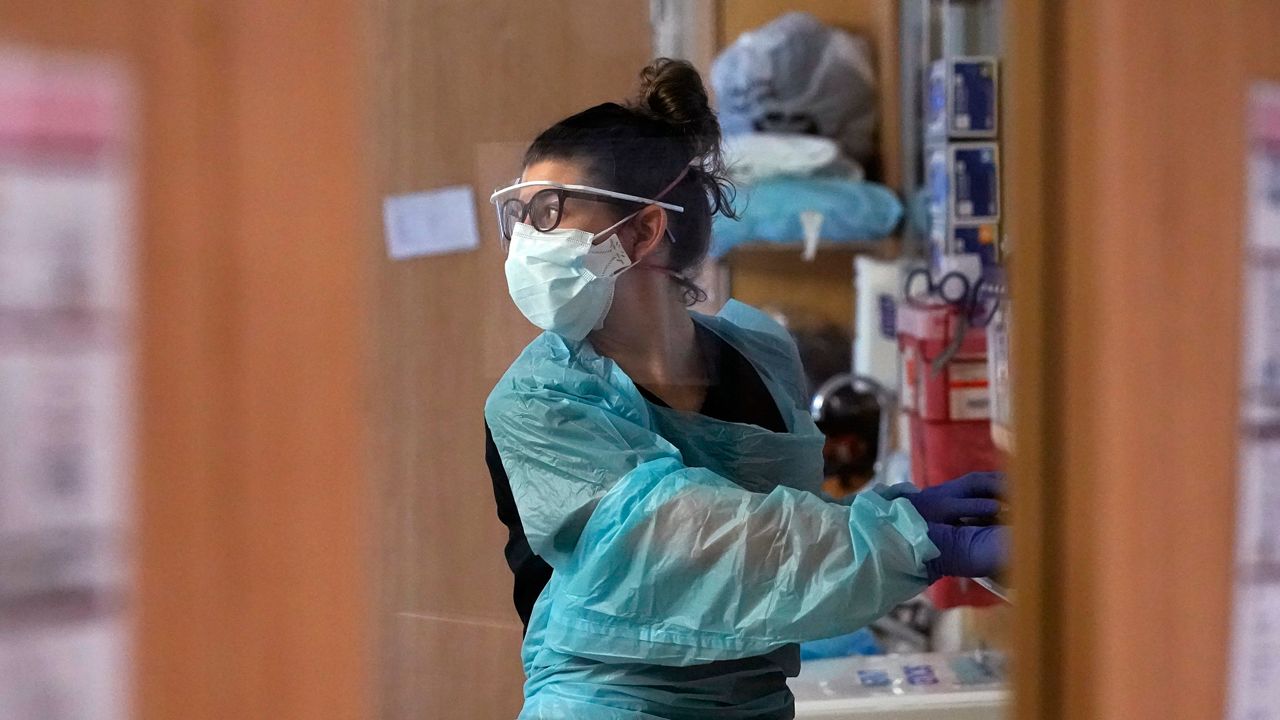
The CDC updated its guidance on face masks last week, encouraging more Americans to seek out the N95 and KN95 masks used by health care workers. Well-fitting respirators like N95s offer “the highest level of protection,” the new guidance states, and filter out the virus more effectively than cloth versions.