WOODRUFF, Wis. — Across Wisconsin, as spring blooms are starting to emerge from the soil, a tiny threat is also popping out of the ground: Ticks, and the disease-inducing bacteria they carry.
“Most people are aware of Lyme disease,” said nurse practitioner Ashley Johnson, who focuses on treating tick-borne disease. “I'm not sure that everyone is aware of how serious it can be if it's undertreated or left untreated.”
What You Need To Know
- Rates of Lyme disease have risen in recent decades, but getting treatment can be a challenge
- The Tick-Borne Illness Center of Excellence in Woodruff provides treatment for patients with new or chronic symptoms
- The debate over chronic Lyme disease is still controversial, which providers say can be frustrating for patients
- Precautions like covering up and checking for ticks every day can help you stay safe during tick season
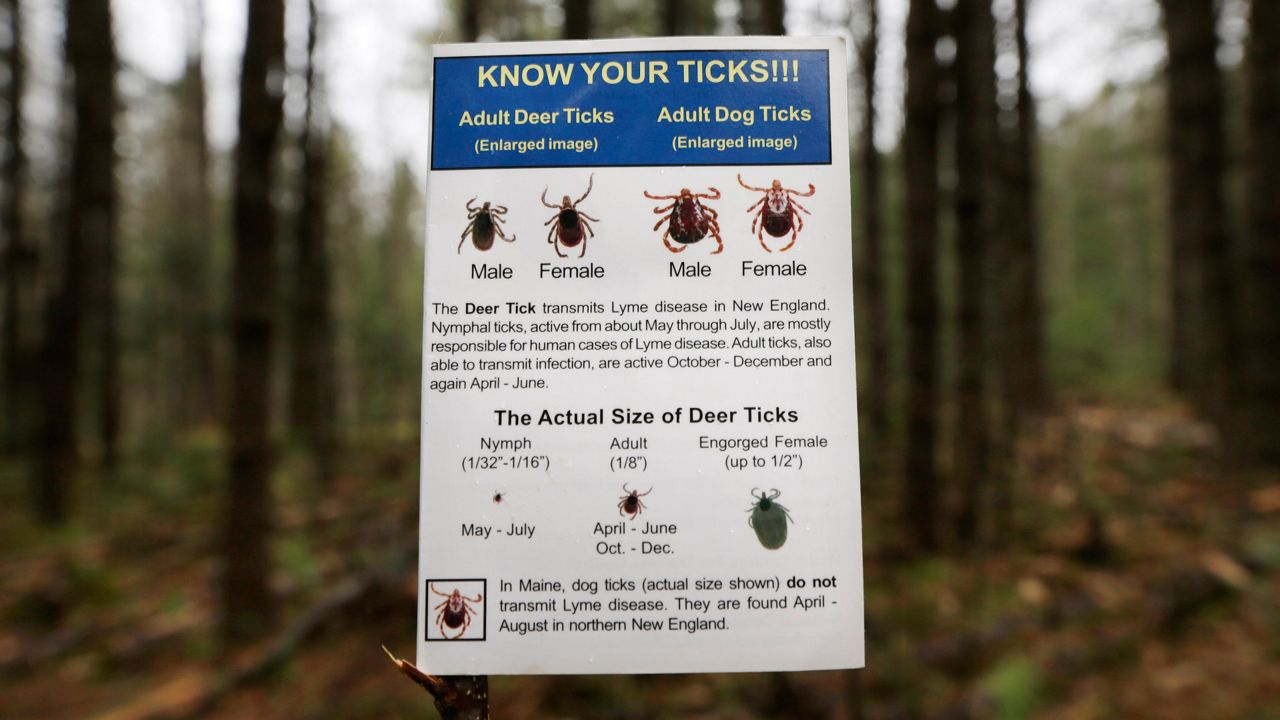
Lyme disease spreads when an infected deer tick bites a human and transfers its disease-causing bacteria, which then can cause symptoms like fever, headache, fatigue and a signature "bullseye" rash. Usually, humans are infected by the tiny, immature ticks known as nymphs — which can be tough to spot, and can latch onto hard-to-see body parts like the armpits and the scalp.
Over the past few decades, ticks have been fanning out across almost every corner of Wisconsin — and bringing higher rates of illness along with them. Wisconsin is one of the leading states in the U.S. for cases of Lyme disease, according to the Department of Health Services, and its numbers have more than doubled in the past 10 years.
But even as more and more Wisconsinites struggle with tick-borne diseases, getting treatment is often a challenge, Johnson said.
The Tick-Borne Illness Center of Excellence, where Johnson works, hopes to fill some of those gaps. The center opened its doors in September 2019 with the support of the Howard Young Foundation, a regional nonprofit, with the goal to provide “hope and healing” for patients, said operations manager Kathy McCaughn.
Since it launched, the center — which is based in Woodruff, an endemic area for tick populations — has treated more than 400 patients, McCaughn said, and hopes to keep growing.
“The bigger our practice gets, the more help we know that we're providing to people that are suffering from a tick-borne illness,” she said.
Chronic Lyme? It’s complicated
In Wisconsin, Lyme disease is the most common illness spread by ticks, the DHS reports. It spreads when an infected deer tick bites a human and transfers its disease-causing bacteria.
And, while many Lyme patients recover quickly with antibiotic treatment, some report persistent symptoms that stick around for much longer. Joint pain, fatigue, headaches, sleep disorders and memory issues are some of the common signs, Johnson said.

But a key issue for these patients is that the medical community is still split on whether the diagnosis of “chronic Lyme disease” even exists, she said. The question of whether Lyme infections can cause months, or even years, of lingering symptoms has long divided experts.
“The first thing that research needs to do is [make it] so that everybody is on the same page with chronic Lyme,” McCaughn said.
On one side — where the Tick-Borne Illness Center stands — some providers think that Lyme disease can cause longer-term infections, and that chronic patients should get treatment for their lingering symptoms, said Johnson, who wrote her master’s thesis about the controversies around chronic Lyme.
On the other side, some providers believe that a patient’s Lyme symptoms should go away after initial treatment with antibiotics, and any lingering problems are unrelated.
“A lot of our patients actually are so frustrated because they're not being heard and they're not being validated,” Johnson said. “They get told that it's not Lyme disease, that it's possibly in their head.”
The symptoms of Lyme disease are not very distinctive, Johnson explained, which leaves many patients to go “undiagnosed or misdiagnosed.” Joint pain, fatigue, headaches, sleep disorders and memory issues are all potential signs — but these problems can also show up as symptoms of other diseases, like chronic fatigue syndrome or fibromyalgia.
The current tests for Lyme disease are far from perfect, too, she said. The two-tier laboratory test looks for antibodies that the immune system produces in response to a Lyme infection. But much like a COVID-19 antibody test, the results can tell you if you’ve been exposed to the virus at some point in time — not whether you are currently infected.
“There's not really an accurate test that really tells you, ‘Yes, you have Lyme disease,’ or, ‘No, you don't have Lyme disease,’” Johnson said.
And the test can turn up false negatives, especially in the early stages of an infection when the body hasn’t built up much of an immune response yet, Johnson said. Some research has shown a Lyme infection can actually suppress the immune system, she added, so in a bit of a catch-22, an infected patient may struggle to build up the antibodies that would get a positive test result.
With these drawbacks in mind, Johnson said the center doesn’t use the lab test as a “rule-out tool,” but as a guide, paired with patients’ reports of their symptoms and possible exposure to ticks.
The center’s staff — which also includes Dr. Samuel Shor, a Virginia-based physician and Lyme expert who sees patients via telehealth — develops unique treatment plans for every patient.
Treatment plans can include antibiotics, herbal supplements and other drug therapies, Johnson said. And sometimes, the providers also need to address co-infections that also get passed on by ticks — like the parasite babesia, which can cause headaches and night sweats, or the bartonella bacteria, which can cause tingling and numbness.

A lot of times, she added, just offering validation for how patients are feeling can make a big difference, especially with all the confusion surrounding long-term Lyme symptoms. She said the center’s staff tries to act as a “quarterback” for patients, advocating for them through the recovery process.
“When they come here, the first step is to hear their story. Hear what they've gone through, really take a listen to their symptoms,” Johnson said. “We like to treat everyone as a whole person, so address each of those symptoms, not just the disease.”
Staying tick-free
Ticks, like humans, tend to start emerging in Wisconsin once the weather gets above freezing.
Usually, ticks are most active from about May to September, according to the DHS, but Johnson said an early melt this year means tick season got an early start.
But if you’re trying to get outdoors, “don’t let that scare you from enjoying beautiful Wisconsin,” McCaughn advised — just take some precautions to stay safe.
Using repellents like permethrin and DEET can help ward ticks away, Johnson advised. Other helpful measures include wearing long sleeves and pants in light colors, to make ticks easier to spot; tossing clothes in the dryer right after getting back from an outing; and checking everyone, including pets, for ticks on a daily basis after spending time outside.
If you do find a tick bite, and especially if you develop a rash or other symptoms, you should get in touch with a provider, she said. Doctors can treat a bite with antibiotics to reduce the risk of developing Lyme disease.
“Preventative is key,” Johnson said. “If it goes untreated, that’s when it causes issues.”
Looking forward, McCaughn said the center is hoping to get back to doing more research about tick-borne illnesses. The team had previously been more involved with collecting blood samples for research, but had to put some of that work on hold during the pandemic, she said.
Johnson said she hopes research can help develop better treatments for those with long-term Lyme symptoms. And, by spreading more awareness and education, she wants more providers to be able to catch and treat tick-borne illnesses early on — so that patients aren’t left suffering through chronic symptoms in the first place.
Though there’s still “a long ways to go” with the challenges for Lyme treatment, the Tick-Born Illness Center staff said they find a lot of rewarding moments in their patients’ journeys — whether it’s helping someone who has been unable to work get back to some of their normal life, or seeing a patient who first came in a wheelchair walk into their latest appointment.
“We understand what they've been through with all this frustration,” Johnson said. “And so, we hope that we can provide for them some positivity and quality back in their life.”