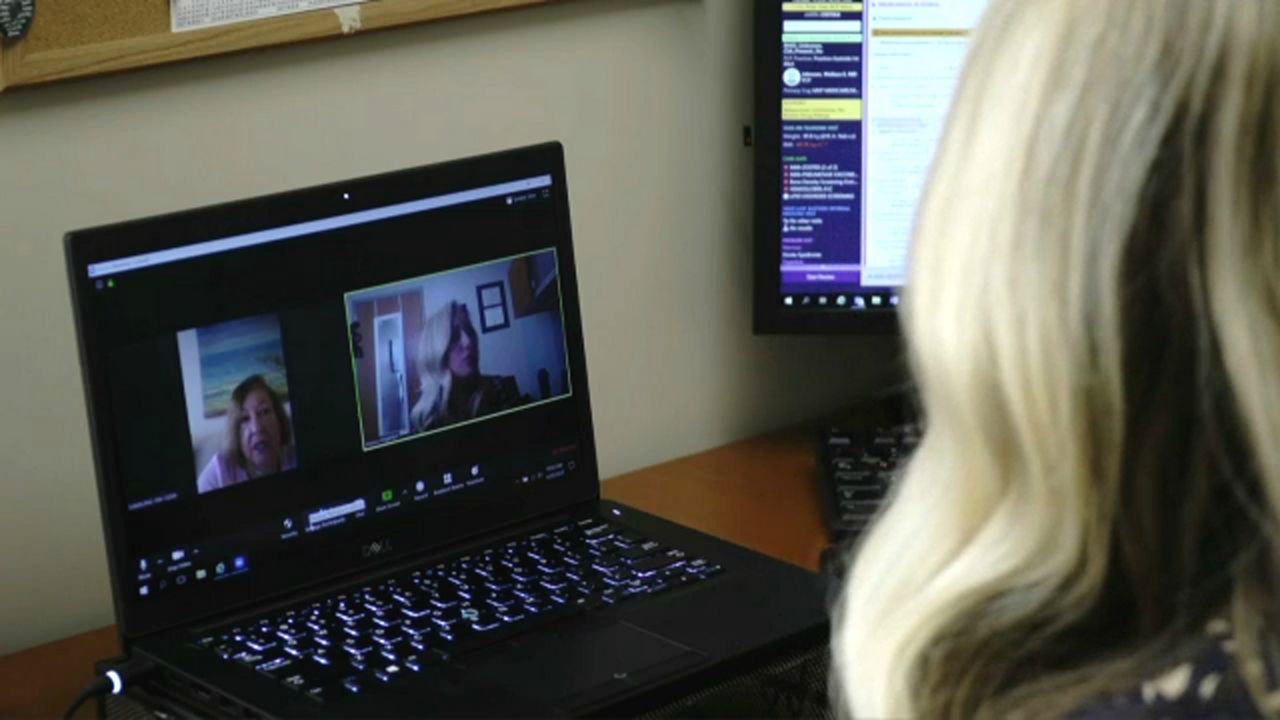
LEXINGTON, Ky. – Telehealth became commonplace during the COVID-19 pandemic, and its popularity has even led to a newly formed coalition pushing to make the practice more permanent nationwide. While the era of health care provided exclusively within the confines of a clinic or hospital confines is likely over, there are some unintended consequences to the telehealth boom.
What You Need To Know
- Kentucky began implementing more telehealth measures in 2018
- House Bill 140 addresses telehealth in the Commonwealth
- Increased cases of fraud have not been a consequence in Kentucky
- Rise of service's popularity during pandemic is the major factor in legislation
“A year into the pandemic, telehealth has become widely accepted,” said Matt Volz, of Kaiser Health News. “Some states are now looking to make permanent the measures that have fueled its growth. But with it have come some unintended consequences, such as a rise in fraud, potential access problems for vulnerable groups and conflicts between out-of-state and in-state health providers.”
Kentucky Medical Association Executive Vice President Pat Padgett said the state began working to make telehealth permanent in Kentucky in 2018, long before the COVID-19 pandemic contributed to the rise in its popularity.
“We're actually one of the leaders in the country for telehealth,” he said. “Kentucky passed a law back in 2018 that provided for payment to providers for providing telehealth; we were one of the first states to do that.”
During its more recent session, the Kentucky Legislature passed House Bill 140, which makes some of the telehealth measures implemented during the pandemic permanent. The bill requires the Kentucky Cabinet for Health and Family Services to establish minimum standards for telehealth. While it does prohibit certain practices, it also requires reimbursement rates for telehealth to be equivalent to reimbursement rates for the same service provided in-person and amends the definition of telehealth as defined in Kentucky Revised Statute 304.17A-005.
“I think one of the most important things the bill does is allow for audio-only telehealth,” Padgett said. “Before the pandemic, to see a provider by telehealth, a person had to go to a specific site that the government approved, and certain things had to happen to be seen that way. The pandemic changed all of that, and people began seeing their providers over Zoom or by phone. I think people began to see it was very accessible and convenient, and they wanted to continue to do that. There are many visits where you will have to see a physician, and you should see a physician, but there are also other visits that can be done by telehealth. I think you will find that a lot of physicians, hospitals, and other providers have integrated telehealth into their normal process, and I just don't think there’s going to be any going back.”
Padgett also said telehealth contributing to an increase in fraud has not been and will likely not be a consequence in Kentucky.
“We do not see an increase in fraud,” he said. “I've heard the argument it's easier for somebody to commit fraud through providing telehealth, but I think it's important to understand that if a physician or any provider sees a patient, to get paid by an insurance company or by the government to see that patient, you’ve got to fill out paperwork, you've got to assign billing codes telling the payer what you did with that patient, and you've got to have documentation to back it up. If somebody is going to commit fraud, that's where they're going to do it. It doesn't matter whether somebody’s in the office or on the internet, they still have to jump through many hoops to do that, and those same hoops exist whether you're in person, over the internet, or on the phone. I don't think that there's any greater risk of fraud than there would be by seeing somebody in person.”
Access to telehealth by vulnerable groups, such as the older populations in rural areas, is also a concern among opponents of expanded and permanent telehealth measures. Still, Padgett said it is not as much of a concern as statistics lead people to believe. The problem is addressed in the legislation by allowing audio-only telehealth visits.
“Internet access for telehealth is not just a problem in rural areas,” he said. “Many of the same problems exist in more urban areas, like certain areas of Louisville and places like that. But internet access is one reason we wanted to make sure audio-only – being able to just talk to a provider over the phone – would still be covered. The new law here in Kentucky was for that very reason. There may be reasons, whether it’s technology or knowledge of technology, that people may not be able to use the internet, so they can just pick up the phone and do telehealth that way. That's one of the reasons we wanted that in there.”
House Bill 140 also permits the Kentucky Department for Medicaid Services to approve other telecommunication technologies for telehealth using federal COVID-19 relief money.
“I think a lot of doctors ran into patients, and not just elderly patients, but a lot of different patients that didn't know how to use the internet for telehealth,” Padgett said. “I think it was a learning experience on both sides, and it will continue to be something of an issue. That just goes back to the point about why we wanted audio-only to be covered as telehealth.”
As for conflicts between in-state and out-of-state providers, Padgett said that is just the nature of health care in Kentucky, which borders seven states and has many people living along those borders.
“It’s interesting to be in health care in Kentucky,” he said. “If you're in Eastern Kentucky, if you're in Ashland, for example, you might go see somebody in West Virginia; if you're in Somerset, you might go to Knoxville; if you're in Hopkinsville, you might go to Nashville; it works both ways. People in West Virginia come over to Ashland; people in Knoxville may come over the border into Kentucky because it's more convenient. There's a lot of cross-border work. I think the one thing that's still required is that if you're a physician or another provider in Ohio, if you're going to see a patient that's sitting here in Kentucky, and you're going to see them by telehealth, you have to be licensed in Kentucky.”
A new lobbying coalition comprised of interest groups and hospital chains called Moving Health Home has formed to make the shift to telehealth more permanent nationwide.
“The telehealth boom has made one thing clear: The era of health care provided exclusively within the confines of a clinic or hospital is over,” said Erin Brodwin of medical news outlet STAT. Making some telehealth measures more permanent is not without opposition; however, some have expressed concerns about overutilization and privacy.
“I think there's the potential some payers were reluctant to support it because they thought that you'd see a lot of overutilization; that people would be calling their doctor or whomever too much,” Padgett said. “I think that during the pandemic, they began to see that wasn't happening. In fact, they wanted telehealth because they wanted people to be seen by their doctor to avoid problems down the line. I'm not speaking for the payers, but I think they've seen that it is certainly a useful way to provide certain types of care. It will keep somebody from going to the emergency room, which is much more expensive for the system and the insurers.”
Federal and state HIPAA requirements for telehealth to be covered by one’s health insurance, such as prohibiting over-the-phone doctor visits to protect privacy, were put aside during the pandemic.
“There's a lot of push right now to keep those requirements loosened up,” Padgett said. “Privacy is critical, but being able to see a physician or another provider when you're sick, not feeling well, or when you think you may have to go to the emergency room might be more important.”



