MILWAUKEE (SPECTRUM NEWS) — It all starts with a stick up the nose.
Well, actually, a sterilized swab — and in the more invasive cases, it reaches all the way to the nasopharynx, the upper area of the throat past the nasal cavity. That’s how clinicians typically collect specimens for COVID-19 testing, explains Jose Navidad, molecular and microbiology diagnostic manager at Wisconsin Diagnostic Laboratories.
But collecting that sample is only one part of the journey of a coronavirus test. Here, we take a look at the scientific knowledge and logistical work that goes into bringing a test all the way to a positive or negative result.
Step 1: The Test Kit
A lot of work has to happen before the tests can even get into the hands of clinicians, explains Kristina Georgakas, manager of communications, marketing, and special projects at Wisconsin Diagnostic.
Early on, “when coronavirus first reared its ugly head,” the lab’s leaders started springing into action to validate testing methods and figure out which vendors could provide them with the supplies they’d need, Georgakas says. There are several ways that coronavirus tests can get approved for use, according to the FDA: Some are given expedited FDA approval for emergency use, while others are developed by individual labs or greenlit by state authorities.
“There's a lot of testing on our end before we actually go live with a test that we would decide to offer to the public,” says April Vaughn, preanalytical services manager at Wisconsin Diagnostic.
As the pandemic has grown and demand for these tests has scaled up, labs have also had to navigate shortages from the vendors who sell testing materials.
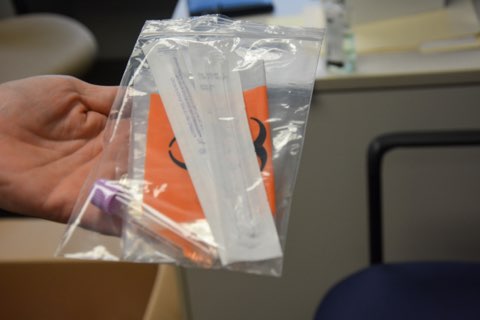
At Wisconsin Diagnostic, they’ve contracted with multiple vendors to make sure they can get enough supplies, Navidad says. While they used to buy test kits fully assembled, these days the vendors are sending them parts separately, leaving lab employees to put the kits together like little goodie bags: two swabs, one biohazard bag, one container with a viral medium (a liquid that helps to stabilize the sample).
“This is something that every laboratory in the United States who’s doing this kind of testing has to deal with, because the supply chain has been strained, to say the least,” Navidad says. “We’ve all had to jump through some hoops.”
Once the kits are all in place, labs send them off to the frontline workers who will administer the tests.
Step 2: Onsite Collection
As demand for COVID-19 testing continues to grow — and some researchers say we still aren’t doing enough — everyone from private practitioners to National Guard members has been mobilizing to help.
“It’s a whirlwind of activity,” says Jonathan Gelfman, clinic director at Shalem Healing in Milwaukee.
He and his team put their test kits to use this week at a pop-up testing site hosted at Bader Philanthropies. Clinicians bustled around to collect more than 150 samples from patients leaning out of car windows or walking up to the outdoor tents.
While some patients come in for the blood-prick antibody tests, many are there for the nasopharyngeal swab — the “brain tickler,” as Gelfman calls it. He says they’ve collected samples from a wide range of people, from those who are experiencing symptoms to others who just want peace of mind.
“You see the gamut of every socioeconomic status, gender, age. You'll see a little bit of everything here,” Gelfman says. “It's truly a frontline activity in combating this epidemic.”
The Wisconsin National Guard has also been conducting tests across the state to support health departments, businesses, and other groups, says Jordan Schultz, a regional officer in charge for the specimen collection teams.
The Guard assigns its teams to different locations based on requests for assistance, Schultz says. Early on, they were geared more toward outbreak responses and targeting certain groups that may have been exposed, he says; now, their “breadwinners” are largely Department of Corrections sites and long-term care facilities.
Similar to other sites, people getting tested move through a series of stations to give their information, consent to the test, and then get swabbed, Schultz says — though the Guard is now using less-invasive nasal swabs that don’t reach as far back. They also launched a digital registration system earlier this month, which has helped them reduce wait times that earlier could drag on for hours.
“It's really a one-stop shop, and that's reduced our errors and increased our throughput,” Schultz says. “We can do upwards of 100 more cars per hour.”
Once the specimen is collected, the transport is key: As the FDA reports, samples must be kept within a certain temperature range to keep the virus alive, and have to reach the lab within 72 hours in order for the test to be accurate. Recently, the National Guard had to toss 142 samples from a site in Iron River after troops overlooked a cooler that was slated for transport to the lab, WPR reports.
Generally, Schultz says the collection teams will place samples in coolers or on ice to keep them between 2 and 8 degrees Celsius — a pretty standard refrigeration temperature. They’ll either drive the specimens to the lab themselves or contract with outside services to get the samples moving on time.
Wisconsin Diagnostics also has courier services to pick up samples and bring them back to the lab, Georgakas says. They have specimens flowing in from clinics, nursing homes, and hospitals all over the state and even as far as Illinois — plus samples from across the Froedtert campus where the lab sits, which shoot in from a system of pneumatic tubes.
Step 3: Back To The Lab
When a specimen returns to the lab, prep teams will get it ready for the testing process. This includes labeling the sample with a number that will follow it through the process so that patient names aren’t directly on display, Georgakas says. Then, it’s time for the scientists to figure out which samples have bits of SARS-CoV-2 — the particular virus at the root of this pandemic — mixed in.
Many coronavirus tests follow a process called a polymerase chain reaction, or PCR. This type of test checks whether the virus’s genetic information is present in the sample, Navidad explains.
(There are also antigen tests that check for proteins on the virus’s surface, but these rapid tests are more likely to miss active infections, according to the FDA. And antibody tests, which use blood samples to see if the immune system has been activated to fight the coronavirus, indicate past exposure instead of diagnosing active infections.)
When a swab comes in, Navidad says, it gets placed in a chemical solution that breaks apart the cells and releases nucleic acids — the DNA or RNA whose unique sequences can help identify what’s in a sample. The novel SARS-CoV-2 coronavirus includes single-stranded RNA, according to the International Atomic Energy Agency, which has to be converted into DNA using specific enzymes in order to move forward with PCR.

From there, the PCR process helps quickly copy the genetic information and flag any matches with viral sequences.
We can think of DNA as two shoestrings wound together in that classic double helix structure, Navidad says. Each strand is made up of a series of building blocks called nucleotides, and the two strands are perfectly complementary.
What PCR does first is to break these two shoestrings apart, leaving single strands floating around in the solution. Then, it injects strands of DNA that are custom-built to match the virus’s unique genetic sequences. If there is viral DNA in the sample, these primer strands will naturally latch onto the complementary strands, “like a Lego piece that just fits perfectly,” Navidad explains.
In this way, each strand of matching viral DNA gets doubled. The series of events — splitting the shoestrings, then letting primers match with them to create more strands — keeps repeating and exponentially increases the amount of viral DNA, so that even tiny amounts of virus in the sample can become billions of copies.
“The whole purpose behind it is to make the testing — that identification of that pathgenic organism — sensitive enough to find that one little particle,” Georgakas says. “It's like a needle in a haystack to start out with.”
When the DNA primers bind with the viral strands in the sample, they also activate fluorescent signals that help keep track of these genetic matches, Navidad says. The process includes chemical compounds with, in essence, a “light” on one end and a “light cover” on the other.
In the process of duplicating the viral DNA, the cover gets clipped off, so the so-called fluoroforms can shine freely as they float around the solution.
“In a sense, every time we create a new strand of DNA, we will create a little unit of illumination,” Navidad says. “The PCR allows us to double strands in every cycle, so you see the exponential growth of two and four and eight and so forth. And the more you create, the more little light units you create.”
Of course, this is all happening at an incredibly small level. The lights, impossible to see with the human eye, are read out by an analyzer that turns each sample into a line on a graph. The more light units detected in a particular sample, the more its line curves upward.
If a sample doesn’t include the virus, then the DNA primer strands won’t have anything to bind to and the lights will stay covered, Navidad says. But if enough lights accumulate to pass a certain threshold level — that signifies a positive test.
Step 4: The Results
At this point in the pandemic, the task of managing all the incoming tests has become an “all-hands-on-deck” affair, Navidad says. When the lab started performing tests in March, they were turning around maybe 50 samples daily; now, they’re working with close to 3,000 tests each day.
This laboratory PCR process tends to take about three to three and a half hours, Navidad says. But as many labs have become backlogged, some wait times for results have shot up significantly. Georgakas says their lab prides itself on keeping its turnaround times short, still returning results in under 24 hours — or even faster for high-priority cases like ER patients or those with respiratory issues.
“It's very rewarding from a scientist’s perspective and from a health-providing organization to be able to reach out to these folks,” Navidad says. “If we are able to reduce extended morbidity or premature deaths because of the turnaround that we are doing, it is a very rewarding thing.”

Schultz says for the National Guard sites, they’ve been achieving strong turnaround times, some in the range of 36 to 48 hours. Whereas before they were calling everyone with results, the new digital system lets them deliver information directly online, which has also sped up the process.
For the Shalem Healing tests, Gelfman says they tell patients to expect a call within one to three days. During this pandemic, he says, giving people this information about their status has become an essential part of the clinic’s mission.
“We're a community-based clinic that's here for our communities,” Gelfman says. “And the goal is to give them enough information by doing this test, so that they themselves, their families, and their communities can be healthy and well.”
Georgakas says Wisconsin Diagnostic is continuing to scale up, looking into training more staff and bringing on additional equipment. Across the state, laboratory testing capacity has continued to grow, with the Department of Health Services estimating more than 24,000 tests are now available each day.
As the COVID-19 pandemic continues — and as more pandemics could pop up in the future — Vaughn says she hopes there will be more visibility for laboratory staff. After all, she says, their work is also a form of patient care.
“We always call ourselves the ‘black box’ of the hospital, but we are an integral part of healthcare,” Vaughn says. “Every single sample that comes into our laboratory is a patient. It’s somebody's mom or grandma or uncle or brother.”



