Before the latest coronavirus case spike started in August, things had seemed to get back to some semblance of normal. Daily case numbers in North Carolina were being counted in the hundreds, not the thousands.
But then the more-infectious delta variant arrived just as the new school year began. Schools started mandating masks and the state’s biggest counties went back to requiring face coverings indoors. Public health officials pleaded with North Carolina’s unvaccinated to go get the shots.
The numbers appear to be subsiding again, according to data from the North Carolina Department Health and Human Services. But how does the pandemic finally end?
The coronavirus vaccines were not a silver bullet. Wearing masks has turned into the latest culture war. Another variant could be on the horizon.
The general consensus from public health officials is that COVID-19 is here to stay. If that’s true, then what does the future look like? What’s the endgame?
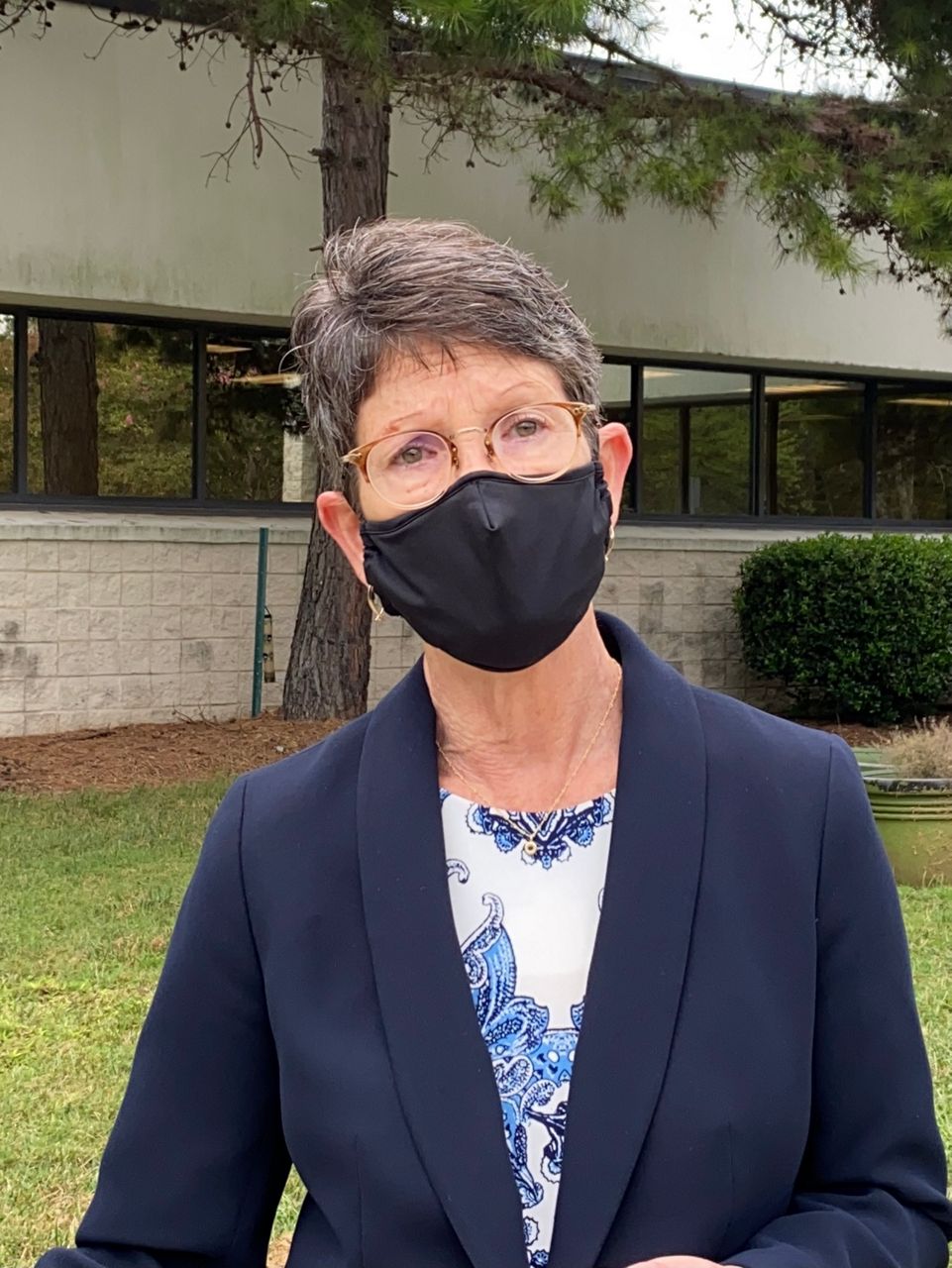
“We can manage it. We can make it less deadly. We can make it easier for the folks with flu-like symptoms,” Mecklenburg County Public Health Director Gibbie Harris told Spectrum News 1 in a recent interview.
“With the flu, if you get the flu, you’re home sometimes for two weeks. You don’t feel good at all,” Harris said. “If we can get to the place where that's acceptable in our society with COVID and people are continuing to do the things that they want to do, I think that’s the endgame. But to get there, we’ve got to get more people vaccinated.”
Dr. David Wohl, an infectious disease specialist at UNC Health, agreed.
“It’s all about the really sick people. If we stop having the really sick people and we’re just dealing with how you get through a week feeling kind of crappy and a box of Kleenex, then I don’t think we’re going to be all freaked out like we are right now. That’s the endgame,” he said.
“Make it like flu. Flu kills tens of thousands of people a year, which is horrible, and largely preventable. But we don’t freak out. We’re freaking out because this is an order of magnitude different,” Wohl told Spectrum News 1.
“The reason we’re freaking out right now is because our ICUs are chock full of people struggling to breathe because of COVID-19,” he said.
To get to that place, both Wohl and Harris said, more people need to get vaccinated and keep wearing masks in public spaces so they don’t get sick.
Wohl said there’s a third piece to the puzzle, too: medicine that can treat people who do get the coronavirus. He pointed to monoclonal antibody treatments, which have proven very effective at keeping people from getting the most serious symptoms of COVID-19.
But monoclonal antibody treatments require people to go in and get infusions. It’s not an easy treatment, but it works, he said.
“Imagine a world where most people are vaccinated, so most people don’t have to face the risk of getting really really sick,” Wohl said. “But if they do get sick, they could take a pill that knocks it out, almost like we have for flu.”
He said there’s a lot of research right now into developing new therapies for the virus, so maybe one day people can just take a pill if they get COVID-19.
The goal, he said, is “this becomes not the threat that we’re dealing with right now, we won’t have our ICUs overflowing, our emergency rooms with people in the corridors because there’s no beds in the hospitals.”
“Vaccine, plus masking, plus easy-to-use therapeutics, that gets us to normal,” Wohl said. “That’s the endgame.”
More and more people are getting immune to the virus everyday. Wohl said people are becoming immune because they either get the virus or get vaccinated, or they get the virus, then later get vaccinated, and now they have what he called “super-immunity.”
Harris, in Mecklenburg County, said she doesn’t think the world will ever be able to eradicate COVID-19.
“What we need to be able to do is manage it, just like we do other viruses. That’s why we have flu shots in the fall, is to help us manage the flu. We don’t get rid of the flu every year, it comes back, it mutates, it changes, and we have to change our vaccine to address the strains we’re seeing,” she said.
“We’re going to see the same thing with COVID, I believe. The challenge is getting enough people vaccinated so we can manage it, so that it’s not creating the surges that we’re seeing right now, so we’re not seeing our hospitals being overwhelmed,” Harris said.



