MILWAUKEE — Over the past two years, the scientific world has seen a steady flow of research updating what we know about the novel coronavirus, SARS-CoV-2, and how it affects humans.
What You Need To Know
- CDC studies found that booster doses were 90% effective at keeping people out of the hospital during the omicron surge
- Some risk factors might be linked with "long COVID," including autoantibodies, high viral levels and Type 2 diabetes
- Moderna's vaccine became the second to get full FDA approval, while Novavax requested authorization for its protein-based shot
- The new BA.2 subvariant is spreading across the country, but vaccines still seem to be effective against it, per early data
Because the virus is so new, researchers are still grappling with many questions about its function. And because of the nature of the scientific process, no single study can completely answer those questions. Instead, new research is constantly challenging our understanding of the pandemic.
Here, we explore some recent studies that have shed new light on the virus.
Boosters kept Americans out of the hospital during omicron surge, CDC reports
Even against new and tricky variants, COVID-19 boosters still pack a punch, according to real-world results. The CDC released studies and data at the end of January showing that even as omicron was sweeping the U.S., booster doses were effective at preventing many severe cases.
One study looked at health records from August 2021 through January 2022, when the delta and omicron variants took over one after another.
In both of these surges, booster doses were at least 90% effective at preventing COVID-19 hospitalizations, the study found — though omicron led to a slight drop in effectiveness compared to delta.
Boosters also cut the risk of a COVID-related emergency room, or urgent care visit by 82% during the omicron surge, the study found.
And the third dose played a key role: On all of these measures, boosted Americans saw a significant bump in protection, compared to those who had two mRNA shots. Those who hadn’t gotten a booster at least six months out from their initial vaccine series only saw around 57% protection from hospitalization, the study found.
Other studies led by the CDC confirmed that boosters made for stronger protection against infection and death during the variant surges — especially for older adults.
In December, unvaccinated adults 65 years, or older were 51 times more likely to be hospitalized with COVID-19, compared to those with additional, or booster doses, according to CDC data.
"I think we have to redefine fully vaccinated as three doses," William Schaffner, a longtime CDC vaccine adviser who was not involved with the studies, told CNN. "I think it's the third dose that really gives you the solid, the very best protection.”
But the booster drive in the U.S. is still lagging behind other countries, as The New York Times reports.
Only around half of Americans who are eligible for their extra dose have gotten the shot, the CDC reports. Under 30% of the whole U.S. population is fully vaccinated and boosted, according to CDC data.
Study suggests four risk factors for developing long-haul COVID-19
After a case of COVID-19, some patients will bounce back quickly. But others will suffer from symptoms for months, or even years. So far, it’s been hard for scientists to figure out why.
In a recent study, researchers monitored hundreds of patients in the months after a COVID-19 diagnosis — and found some common threads in who was dealing with long-term symptoms.
The scientists identified four possible risk factors they say could be linked with “long COVID.” Out of the patients who were still dealing with symptoms two to three months after they first got sick, nearly all of them had one or more of these factors.
One of these factors was having a higher viral load at the start of a COVID-19 illness — measured by having a high level of coronavirus RNA in the blood. It’s possible that having more SARS-CoV-2 virus to start with can make it harder for the body to fight off the infection, which may lead to longer-lasting health issues, some scientists suggested.
“It makes sense that a higher viral load can equal more symptoms,” family physician Beth Oller told Verywell. “If you have a more severe infection, it is going to take the body longer to clear the virus, which is one thought as to why a higher viral load is correlating with a higher risk of long COVID.”
Another possible risk factor: Having Type 2 diabetes as an underlying condition. Diabetes can weaken the immune system and make patients more vulnerable to infections in general.
Researchers also suggested the reactivation of the Epstein-Barr virus could be a risk factor. Many people catch an EBV infection when they’re young, and then see the virus become latent in the body — still around, but inactive. In the study, though, a number of long-haul patients saw the Epstein-Barr virus become active again.
And finally, the study pointed to the presence of certain autoantibodies — immune fighters that mistakenly attack the body’s own tissues — as the fourth potential risk factor.
Scientists have speculated for a while that long COVID-19 might have to do with an immune system overreaction, rather than the actual virus still lingering in the body. These kinds of misguided immune attacks are at the root of disorders, like lupus and arthritis.
Out of the four factors they identified, autoantibodies were shared between the most patients, study author Jim Heath told The New York Times: Around two-thirds of those with lingering symptoms also had the autoantibodies that researchers were looking for.
There’s still a lot more to learn when it comes to long COVID-19, and scientists emphasized that this study was just the beginning. Figuring out the root causes of long-term symptoms will be key to helping treat patients.
“Once you can measure something, then you may be able to start doing something about it,” Heath told The New York Times.
Novavax looks to enter the vaccine pool — and Moderna gets another vote of confidence
More than a year into the COVID-19 vaccine rollout, another company is hoping to get its shots into Americans’ arms.
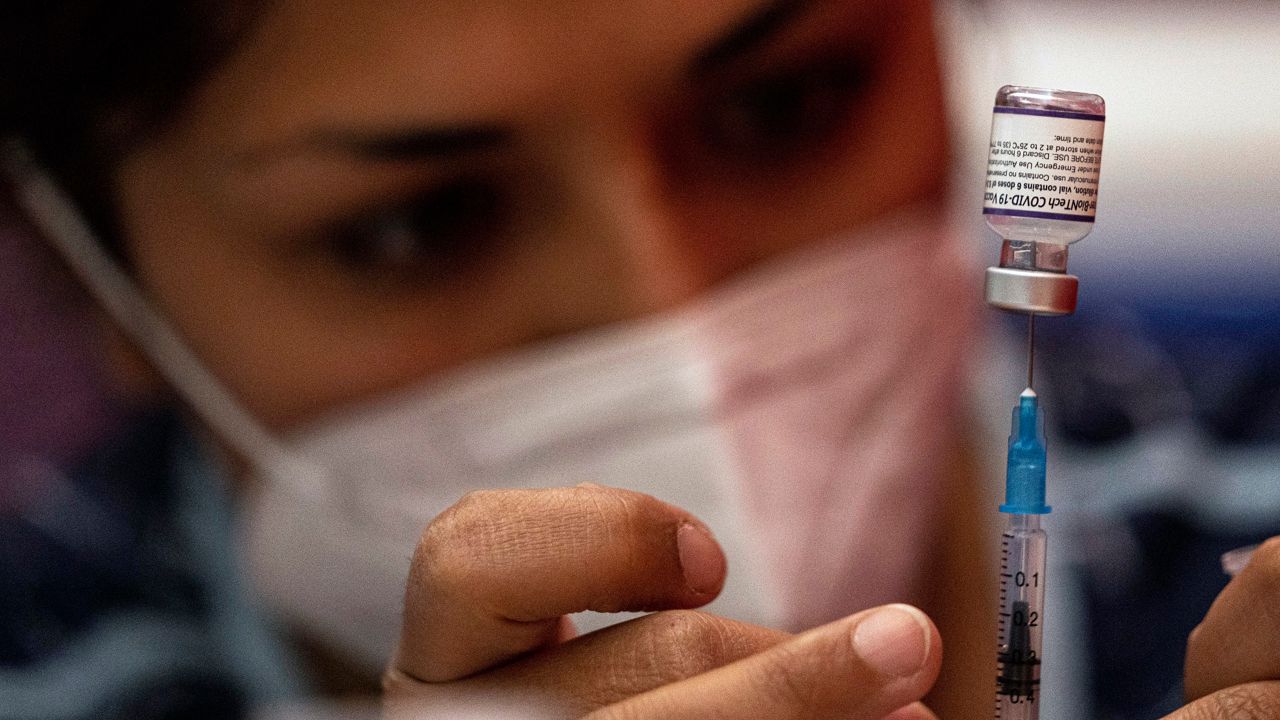
The vaccine effort in the U.S. has, so far, only authorized shots from Pfizer, Moderna and Johnson & Johnson. But earlier this month, the pharmaceutical company Novavax applied for FDA authorization for its own COVID-19 vaccine, which showed promising results in clinical trials.
Like the Pfizer and Moderna vaccines, the Novavax version requires two doses for the initial series, spaced three weeks apart. And its protection seems to be pretty on par with these vaccines: The Novavax version was more than 90% effective in clinical trials.
Unlike Pfizer and Moderna, though, the Novavax shot doesn’t use mRNA technology. It’s based on a “protein subunit” model: Researchers grow tiny particles in the lab to look like the coronavirus’s spike protein so that the body learns to recognize the intruder.
This type of vaccine is already common for routine immunizations, and some experts said it could be a useful option for those who are wary of mRNA shots (though the mRNA vaccines are also shown to be safe and effective).
Stanley C. Erck, president and CEO of Novavax, said in a press release that his team hopes to offer “an alternative to the portfolio of available vaccines to help fight the COVID-19 pandemic."
In other vaccine news, Moderna’s shots got an extra vote of confidence from federal health officials this month. The FDA upgraded Moderna’s vaccine to full approval, after the shots had originally rolled out under an Emergency Use Authorization — a decision that was also backed by the CDC.
Moderna’s vaccine — now know as Spikevax — is the second COVID-19 shot to get FDA approval, after Pfizer’s version got the full green light in August.
It’s a technical change, but one that gives some more freedom in how the vaccine can be used and marketed, as well as confirming health officials’ confidence in the shots. The CDC’s vaccine advisory panel agreed unanimously that based on all the data so far, the benefits of Moderna’s vaccine outweighed any risks.
"We now have another fully approved COVID-19 vaccine," CDC Director Rochelle Walensky said in a statement. "If you have been waiting for approval before getting vaccinated, now is the time to join the nearly 212 million Americans who have already completed their primary series.”
More news to note:
The omicron subvariant BA.2 has now shown up across the U.S., and made up a little under 4% of all new cases, according to the CDC’s latest estimates. There’s still a lot to learn about the new, and potentially more contagious, version of the virus, but early research suggests our current vaccines still protect against the subvariant.
A study found that lions at a South African zoo were sick for weeks after contracting the coronavirus from their handlers, raising more concerns about the virus’s spread in the wild — and its potential to spread back to humans. Other species have been shown to catch the virus in the past, including white-tailed deer and house cats, but most haven’t shown serious symptoms.
Tens of thousands of tons of medical waste have been piling up around the world during the COVID-19 pandemic, according to a new report from the World Health Organization. From test kits and syringes to masks and gloves, the waste adds up to a big burden on waste facilities and a significant threat to the environment, the WHO analysis found.