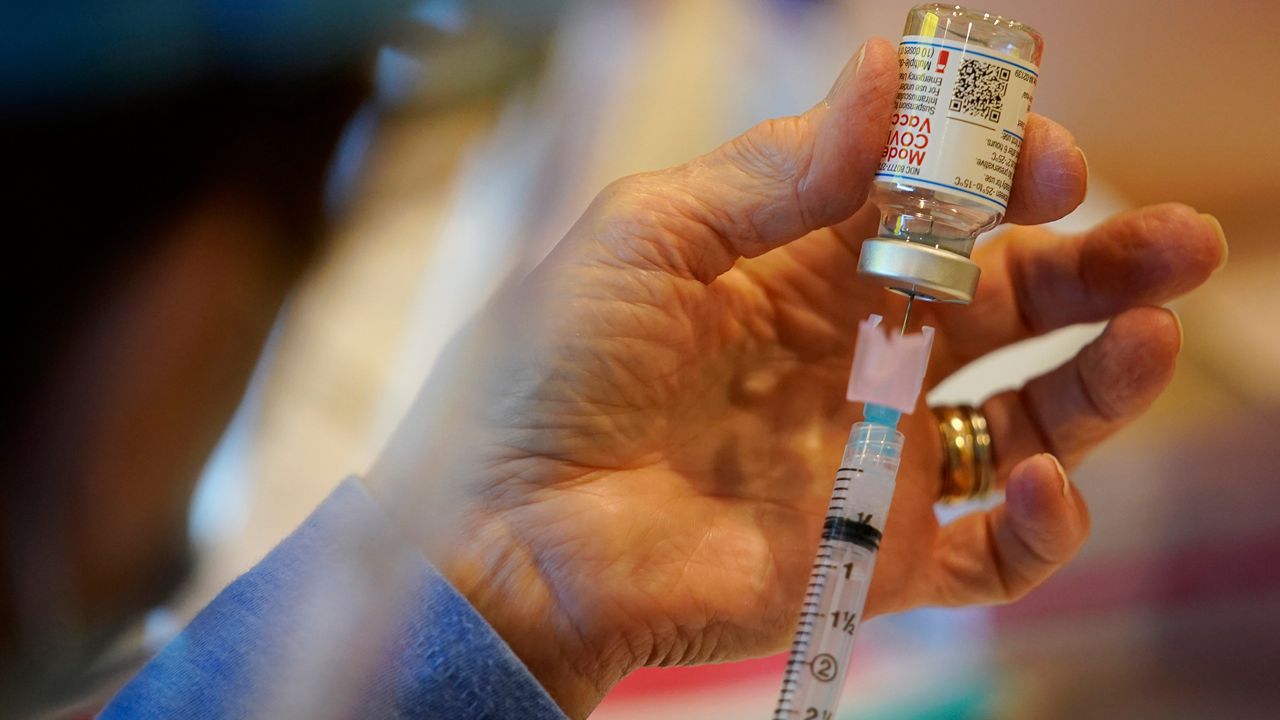
A committee of independent advisers to the Food and Drug Administration voted on Thursday to recommend booster shots of Moderna’s COVID-19 vaccine for Americans 65 and older and other high-risk groups at least six months after a second dose.
What You Need To Know
- A committee of independent advisers to the Food and Drug Administration voted on Thursday to recommend booster shots of Moderna’s COVID-19 vaccine for Americans 65 and older and other high-risk groups
- The panel voted unanimously to recommend boosters of Moderna's COVID-19 vaccine for people 65 and older and adults 18 and up with underlying medical conditions that put them at high risk of severe COVID-19 and those with occupation exposure
- The Vaccines and Related Biological Products Advisory Committee listened to presentations from the FDA, Moderna and others before debating and then voting on whether additional doses of the vaccine should receive emergency use authorization
- The panel will meet again Friday to discuss booster shots of Johnson & Johnson’s vaccine
The Vaccines and Related Biological Products Advisory Committee listened to presentations from the FDA, Moderna and others before debating and voting on whether additional doses of the vaccine should receive emergency use authorization to counter waning effectiveness.
The panel voted unanimously to recommend boosters of Moderna's COVID-19 vaccine for people 65 and older and adults 18 and up with underlying medical conditions that put them at high risk of severe COVID-19 and those with occupation exposure.
Notably, the panel recommended a lower dose of the vaccine – a half-dose booster – for the third shot to boost protection from the virus.
Their vote is not binding, but will play heavily into the FDA’s final decision. Next week, a panel convened by the Centers for Disease Control and Prevention will offer more specifics on who should get one.
The FDA panel will meet again Friday to discuss booster shots of Johnson & Johnson’s vaccine.
Dr. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, told members that “separating waning effectiveness from reduced effectiveness against the variants such as the delta variant can be challenging. And ... the vaccines are still very effective against serious outcomes, such as hospitalization.”
On Tuesday, the FDA released a mixed analysis of Moderna’s data. Agency scientists found that a 50-microgram third dose – half of what was administered in earlier shots – elevated the level of antibodies at least six months after initial inoculation. However, the data do not clearly demonstrate a booster shot is needed, the scientists said.
“Some real world effectiveness studies have suggested declining efficacy of Moderna COVID-19 Vaccine over time against symptomatic infection or against the Delta variant, while others have not,” the analysis says. “However, overall, data indicate that currently US-licensed or authorized COVID-19 vaccines still afford protection against severe COVID-19 disease and death in the United States.”
In fact, scientists emphasize that all three vaccines used in the U.S. – the ones produced by drugmakers Moderna, Johnson & Johnson and Pfizer-BioNTech – still offer strong protection against severe COVID-19 cases. The issue is how quickly, and how much, protection against milder infection may wane.
What's the evidence that the Moderna vaccine's protection is waning? As the delta variant surged in July and August, people who were more recently vaccinated had a 36% lower rate of “breakthrough” infections compared with those vaccinated longer ago, Moderna's Dr. Jacqueline Miller told FDA's advisers.
Moderna said the single 50-microgram shot should be enough for a booster and would trigger fewer uncomfortable shot reactions such as fever and achiness while also leaving more vaccine available for the global supply.
A study of 344 people found the booster shot six months after initial vaccinations restored virus-fighting antibodies to levels seen after recipients' last dose — and that included large jumps in antibodies able to target the delta variant, Miller said.
Pfizer and Moderna booster shots for immunocompromised people have been approved since August, and one question that came up early in Thursday’s meeting was whether a vote to authorize the vaccines at 50 micrograms would supercede the existing approval for the immunocompromised to receive a 100-microgram third dose.
Marks acknowledged the FDA must clarify that the dosage will remain 100 micrograms for immunocompromised people. FDA officials suggested a fourth, 50-microgram dose for such individuals might be possible, but Marks cautioned: “This is far enough in the future that I don't want to make a definitive statement here. It's something that we do, though, have to cover when we reissue our fact sheets.”
The FDA just went through this process last month in deciding whether boosters of the Pfizer vaccine should be green-lit. The agency followed the advisory committee’s recommendation in authorizing the additional doses for people who are 65 or older, are at an increased risk for severe COVID-19 or work in high-risk settings, including health care workers.
In the next step in the process, a panel convened by the Centers for Disease Control and Prevention recommended the shots for people 65 and older as well as those with underlying medical conditions, but not for people with occupational exposure. However, in making the final call, CDC Director Dr. Rochelle Walensky partially split with the advisers by recommending boosters for all three groups.
At Thursday’s FDA committee meeting, the question of employees in high-risk settings came up again. Dr. Cody Meissner of Tufts University School of Medicine said he believed the panel intended to only recommend booster shots for people whose jobs put them at high risk of contracting severe disease, rather than just infection.
“And I worry because that's been interpreted as, for example, a person who bags groceries at a at a grocery store,” Meissner said. “And, to me, that wasn't quite the intention of what we discussed during the last meeting.”
A. Oveta Fuller, a virologist and viral pathogen researcher at the University of Michigan, however, said she did intend to protect employees such as supermarket workers.
“They're certainly at higher risk for exposure and I, for one, am grateful that we have that allowance, that someone who would like to get the booster is able to do so,” she said.
Marks said committee members will have the opportunity to discuss whether “to refine what we have” but seemed to urge uniformed rules across the various vaccines to prevent confusion among the public.
Just as they did during the Pfizer meeting, Israeli health officials presented data from their booster campaign, which began in July. The research found that infection rates were about 10-fold lower across all age groups in people who received the booster shot compared to those who only received two doses. Severe illness rates were as much as 22-fold lower.
The data were largely based on the Pfizer vaccine, which, like Moderna’s shots, uses mRNA technology.
Dr. Sharon Alroy-Preis, director of public health services at the Israeli Health Ministry, also said officials are not seeing more adverse events than what was observed with second doses. She said cases of myocarditis in young males have been “really rare” and “mild in most cases” with booster shots, but she conceded that there have been some concerns that some young males might be avoiding the boosters.
The FDA in June added a warning to the Pfizer and Moderna vaccines after the CDC found heart inflammation in adolescents and young adults was linked to the shots. Health officials, however, said the cases were extremely rare, that patients generally recover from the symptoms and that the benefits of the vaccines clearly outweigh the risk.
Moderna's booster study wasn't large enough to spot such a rare risk.
The Associated Press contributed to this report.