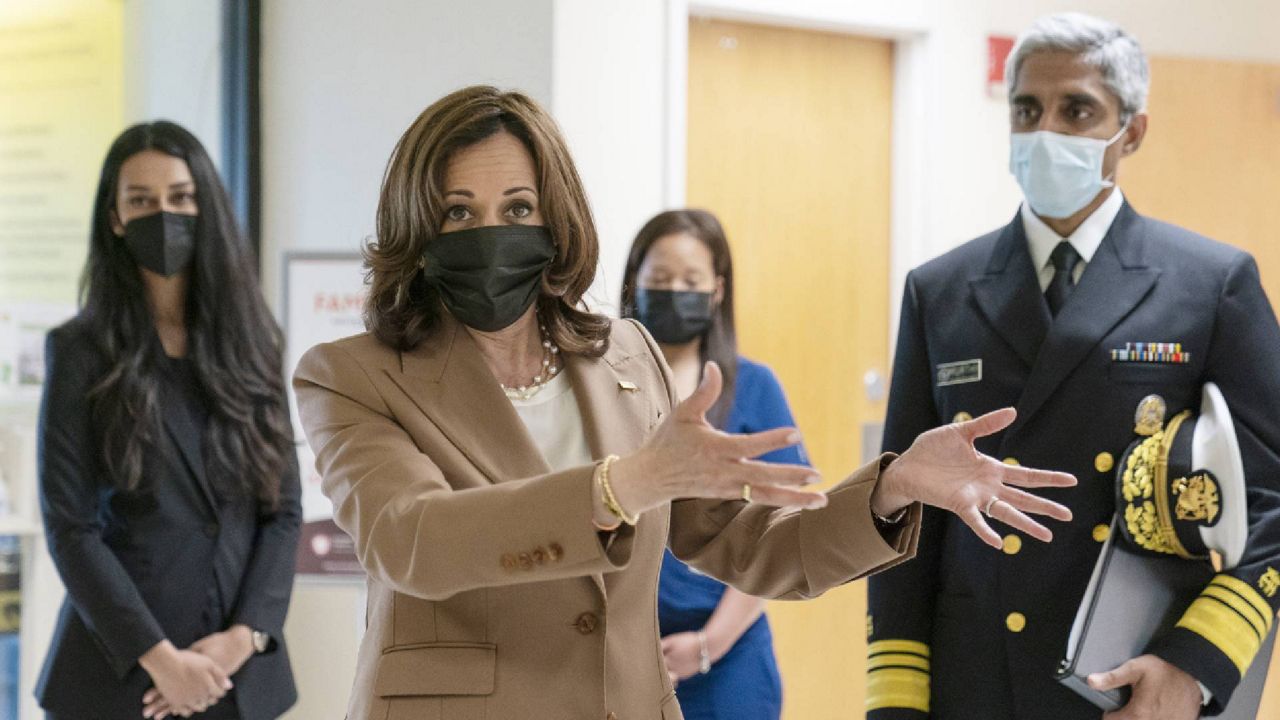
Vice President Kamala Harris and Surgeon General Vivek Murthy on Monday toured a children's hospital in Washington, D.C. to highlight a new federal advisory that calls attention to health worker burnout and makes recommendations to improve those workers’ mental health, with hopes of easing staff shortages expected in the coming years.
The VP and Dr. Murthy met with nurses and staff at Children’s National Hospital about their personal experiences with stress and anxiety as more than 50% of health workers have reported symptoms of at least one mental health condition since the pandemic began, according to the Centers for Disease Control and Prevention, including post-traumatic stress disorder (PTSD).
"If you knew someone who broke their arm, you would help them. You would make sure they went to the hospital to get a cast," Harris said. "We have to do the same when it comes to mental health. I think for too long our system has failed to understand the significance of this."
The “Surgeon General’s Advisory Addressing Health Worker Burnout” released Monday outlines how the pandemic has exacerbated high levels of burnout among medical workers, and it calls addressing the well-being of those workers a “priority” for the Biden administration. Advisories “are reserved for significant public health challenges that need the American people's immediate attention,” according to the release.
"We have asked so much of you over the course of these last two-plus years. Some of you held the hands of those who were dying on behalf of their loved ones," Harris told health workers Monday. "So there is an urgent need that we have, I believe, to address all of this."
Murthy’s advisory also points to burnout as a core factor in a projected shortage of 3.2 million lower-wage health workers over the next five years, such as medical assistants, home health aides and nursing assistants. The report concluded that New York and California will feel the most impact, especially when it comes to home care.
The shortages will also extend to doctors and nurses, the advisory warns: more than 500,000 registered nurses are expected to retire by the end of 2022, and the U.S. Bureau of Labor Statistics projects that will create a need for 1.1 million new RNs across the U.S. Plus, the Association of American Medical Colleges (AAMC) projects that demand for doctors will continue to grow, leading to a shortage of 54,100 to 139,000 physicians by 2033, “with the most alarming gaps occurring in primary care.”
On Monday, Children's Hospital nurse Monique Cauley said she has witnessed her colleagues "work around the clock skipping lunches to care for unstable children" and "continue to keep each other afloat through laughter, hugs and small talk."
Harris and Dr. Murthy on Monday also noted that health workers were already experiencing “crisis levels” of burnout prior to the pandemic, impacting about half of nurses and doctors and even more residents and medical students.
"Addressing health worker burnout is also about more than just health. It's about reflecting the deeper values that we aspire to as a society, values that guide us to look out for one another and to support those who are doing the same," Murthy said at Children's National on Monday.
"Health workers have had our backs during the most difficult moments of this pandemic. It's time for us to have theirs," he added.
The surgeon general’s advisory makes recommendations to fight that burnout, including:
Make the workplace responsive and open to workers’ needs and feedback
Eliminate punitive policies for seeking mental health and substance use disorder care
Make the workplace supportive by providing living wages, paid sick and family leave, rest breaks, evaluation of workloads and working hours and ensuring adequate staffing
Prioritize protecting health workers from workplace violence and ensure that they have sufficient personal protective equipment
Reduce administrative work so health workers have more productive time with patients and colleagues
Prioritize social connection and community as a core value of the health care system
Diversify and expand the public health workforce and improve disease surveillance systems to help address social factors of health inequities and counter health misinformation
The COVID-19 relief bill allocated more than $100 million to reduce burnout and promote mental health among the health workforce, and the CDC also kicked off an effort in November to address health worker burnout, which includes improved data collection, mental health screenings, better training and increased communication.